Insurance is very helpful for binary risks – your boat is either floating or sank, your house either burned or did not. A binary model for health care embeds this implicit bias. It requires a diagnosis – you either have “X” disease, or you do not. This binary approach to health accommodates the “reimbursement for services” infrastructure of our health care system at the cost of an inherently flawed model of health and well-being.
We are not either well or sick. Our bodies and psyche participate in a continual process of adaptation – more or less successfully. The symptoms we experience are the effect of adaptation – either transitory as we accommodate a new optimized state or persistent as we converge towards, but not attain well-being. Optimized well-being is not a static state – it is very much a moving target as we adapt to changing environments, activities, nutritional sources, stress levels, etc. We do not recover from illness, but rather adapt to a new internal challenge. This perspective differs foundationally from the binary sick/not sick healthcare insurance-based framework within which we seek to persist.
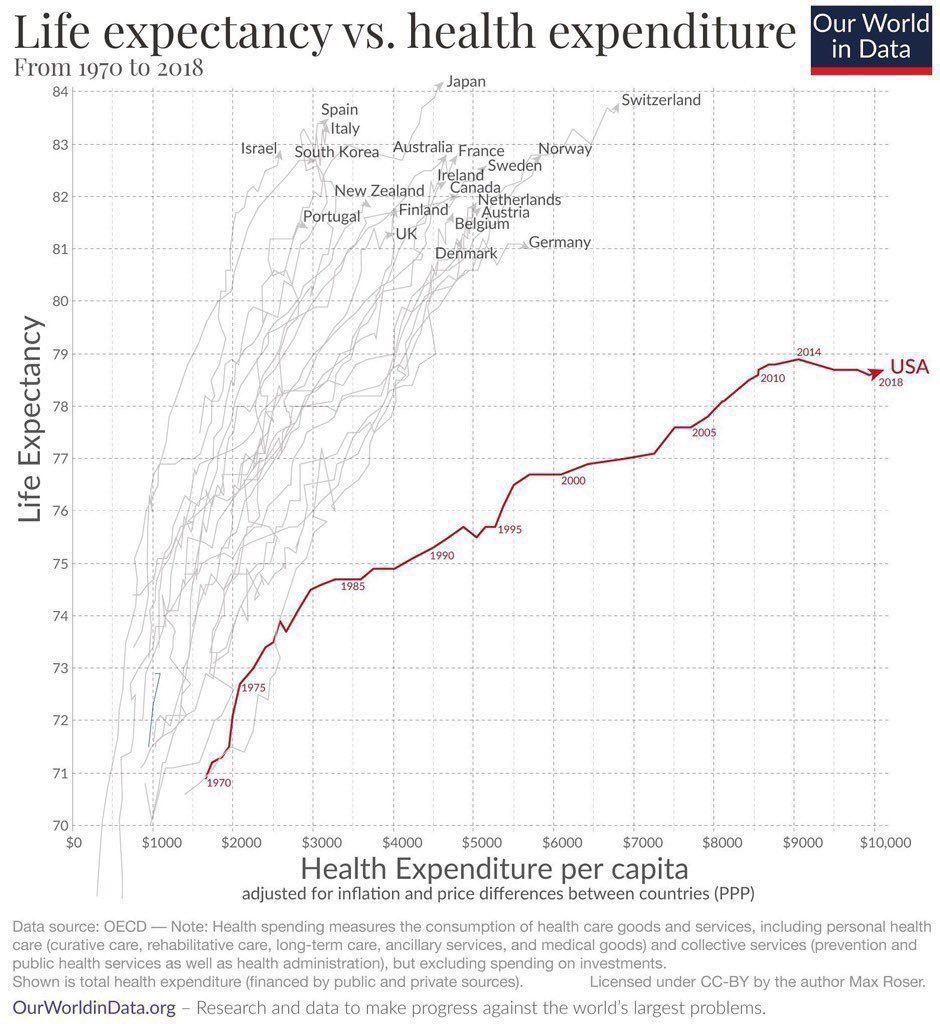
The primary “trip hazard” in this binary model of care is that we easily surrender our agency to a third-party “expert” who, based on their assessment (lab work/Xrays/biopsy, etc.), decides our course of treatment. I must note here that I have profound respect for the scientific underpinnings of medicine. Where I think we fall short is in the framework of their implementation. The binary nature of this framework is observed to have a negative influence on self-responsibility and agency. We behave as we wish until we get sick, and the doctor then, hopefully, fixes us. The framework, at least historically, encourages us to ignore our health or be guided by simplistic metrics for well-being until a symptom emerges that cannot be ignored. If we are underinsured we pray not to get sick. The repercussions for such a strategy can be observed in the above graph, where our health care return on investment is abysmal.
Before the 1920’s the medical care options looked very different, with a more diffuse/competitive range of health care resources and much greater consumer autonomy, and a coincident consumer requirement for self-responsibility. This cornucopia of offerings was crushed by J. D. Rockefeller’s “philanthropy” that institutionalized health care tactics and successfully lobbied to categorize “non-medical” treatments as illegal. Due to the benefits of the economies of scale inherent in this model it was widely adopted in industrialized countries. However, in countries with the single-payer model, the drive to minimize overall cost has counterbalanced this tendency towards Allopathic monopoly. For example, Osteopathy is widely practiced as a first-line treatment of musculoskeletal issues in many countries, where it, although more labor-intensively, resolves most aches and pains complaints, avoiding the common progression to high-cost surgical interventions. In the U.S., we doubled down on this assembly line model of care, driven by the health care insurance industry lobbying efforts. If there is not an insurance code for your adaptive profile, your issue is neither diagnosable nor treatable.
Based on the data presented above one might posit that a major cause of death in the US is the health care system. A single-payer system appears to offer better outcomes. Going even further, it is likely that a system encouraging agency and autonomy, and that can evolve based on the outcomes of traditional/alternative/complementary care options weighted against Allopathic tactics will improve lifespans. A system integrating machine learning with stringent privacy guardrails seems likely to underpin health care providing the best possible health outcomes.